Women’s Health: Building a Comprehensive Approach to Cardiovascular Care in Women's Health
Authored by: Suchismita, Das, Senior Industry Analyst, Healthcare & Life Sciences (HLS) Growth Opportunity Analytics,
Frost & Sullivan
Heart Disease Expands Beyond “Men’s Disease”
Long gone are the days when heart disease was termed “men’s disease”. Which disease is the No. 1 killer of women, globally? It’s no more breast cancer - it is cardiovascular disease (CVD) or heart disease. 35% of all deaths in women, worldwide are caused by cardiovascular disease. Although many people now know that
women face different symptoms before a heart attack and while suffering from CVD, there remains significant room for innovations and improvement in aspects of CVD in women.
CVD mortality has been consistently rising in both men and women, and it is no longer a 50+ years disease. It is disproportionately affecting younger as well as midlife women. Women aged 25-45 are predicted to have significant cardiac disease risks by 2030, making it the biggest set of patients. 1.9 billion women deaths across the world will be due to heart disease in 2030 if left unaddressed today. As CVD comprises nearly 35% of all deaths worldwide, making the disease the leading non-communicable cause of mortality in women. Asia is the region with the maximum prevalence of cardiovascular diseases amongst women. For instance, China has witnessed a 10% increase in women’s heart disease prevalence. High blood pressure is the most important risk factor globally contributing to CVD mortality in women.
Life transitions in women, such as in pregnancy and menopause, can effectively impact heart health. Heart disease is significantly different between females and males in terms of variation in biology (for instance, the size of blood vessels), symptoms, and risk factors. In women, hormones play a substantial role in affecting blood pressure levels due to increased sodium and water retention in the kidneys.
Under-Representation of Women in Cardiovascular Research
Heart disease in women is ‘under’ everything – it’s under-studied, under-recognized, under-diagnosed, under-treated, and under-represented. Women have historically been excluded from cardiovascular research, although efforts have been undertaken to increase women's inclusion and participation. Recent estimates achieved from clinical trials still exhibit an underrepresentation of female participants in heart/cardiovascular research, specifically in research related to coronary artery disease and trials on heart failure.
Approximately, only 35% of female participants are included in clinical trials for chronic conditions such as cardiovascular diseases. In terms of research dollars spent, out of 2 billion for heart diseases, only 20 million dollars are spent on women’s heart health projects –it’s a comparison of 17 cents spent per woman versus 4 dollars per man[1]. This disparity needs to be addressed quickly. The need for 2030 is an ecosystem of gender-specific care – women-specific care. When clinical research and trials are done on men and the findings are applied to women unequivocally, here lies the biggest problem. It needs a lot of catching up to do.
Women’s Heart Disease Care Continuum
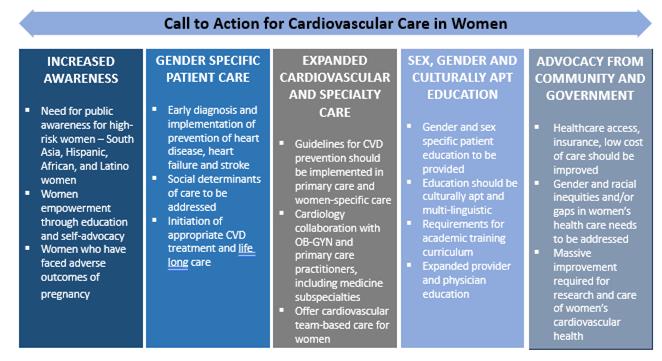
Care and treatment pathways for CVD in women are gaining traction in developed nations where gender-specific care and treatment have recently been introduced in their early stages. However, the scenario in developing nations remains quite underdeveloped - heart diseases in women are mostly treated in primary care settings, lacking the latest screening devices and trained GPs. This technology lag thwarts the early diagnosis and prevention of the disease at an early stage. Women’s cardiovascular care remains suboptimal, with considerably poorer outcomes than in men. Over the last two decades, CVD in women gained a substantial increase in research and publications to address sex-specific symptoms, risk factors, pathophysiology, prevention, diagnosis, and treatment in inequities of care. Approach to address these global inequalities, and to allow a comprehensive approach to cardiovascular care for women, there has been the worldwide establishment of specialized centers offering cardiovascular care for women throughout the lifespan across different ages. The current goal of the global “cardiovascular care in women” community is to delineate an actionable roadmap to implement the vision for equity in offering sex-specific care and to ensure cardiovascular healthcare
access and quality treatment. The entire CV care continuum needs to be modified as per the needs, symptoms, risk factors, diagnosis, and treatment relevant to
women.
For instance, pregnancy symptoms can be early predictors for future health complications in women, so there is a need to build a strong pregnancy care system. In case of pregnant women with diabetes and hypertension keeps suffering from the diseases throughout their life. So there needs to be longitudinal studies to study and predict population health.
Noncommunicable diseases (NCDs) remain the leading cause of mortality in the GCC countries, including CVD, diabetes, cancer, and chronic respiratory diseases in the four major disease groups accounting for nearly 80% of all deaths due to NCDs[1]. Coronary heart disease (CHD) remains the primary cause of morbidity, mortality, and disability in the GCC region. In this region, women patients with CHD are mostly at younger ages at presentation with worse diagnoses. The increasing rate of diabetes leads to a two-fold increased risk of stroke and ischemic heart disease, leading to many other complications and premature death. As GCC countries present the highest rates of lifestyle-related risk factors for NCDs (such as obesity, high caloric diet, and physical inactivity), there have been NCD preventive measures implemented by the GCC countries over the last few years. Periodic screening programs, specifically for women as they get neglected the most, have become national guidelines. Moreover, poor patient awareness, limited access to CVD care, and ineffective preventive strategies for the disease hamper the care protocol. The healthcare systems in the GCC countries have evolved and substantially grown over the last few years, including gender-specific care for women. It is required that all stakeholders involved in healthcare in the GCC should start treating women’s cardiovascular health as a priority and work together to develop and execute strategies to tackle the CHD burden in the region.