The Digital Operating Room: Future of Surgery
Insights By: Dr. Bejoy Daniel, Senior Industry Analyst – Healthcare & Life Sciences, Frost & Sullivan.
Globally, hospitals and health systems face financial pressure due to the associated high operating and administrative costs, declining revenue and reimbursement rates, and the increasing costs of medical devices and infrastructure. The COVID-19 pandemic has further intensified this financial crisis as patient volumes had dropped and negatively impacted revenues further. Despite these challenges, a number of hospitals invested in technology to ensure improved operational efficiency and patient outcomes. Several foundational shifts were seen, including the consumers’ increasing involvement in healthcare decision-making, increasing adoption of virtual health and digital innovations, and the criticality of interoperable data and data analytics use. The main driver of this shift came from the increasing pressure on healthcare providers, governments, payers, and other stakeholders to quickly adapt and innovate.
Significant changes are expected to transform the healthcare landscape for health insurers and providers in the next few years due to the expected shift toward value-based care and the provision of care outside of hospital settings. A number of surgeries and diagnostic procedures that historically required an inpatient hospital stay are now being considered as a possibility of being performed more safely and efficiently in an outpatient setting. More outpatient care centers are being made available through ambulatory surgical centers and patients’ homes. Transformation on a global scale results from clinical innovations and an increased focus on improving the quality of care and clinical outcomes. The growing demand for value-based payment models to reduce the cost of care and improve the overall patient experience is the main factor influencing this shift. This will drive payers and providers to analyze changing patient demographics, consumer preferences, and satisfaction trends to ensure healthcare settings are prepared for outpatient settings. Healthcare settings are strategizing to grow capacity and infrastructure for outpatient services by investing in innovative technologies with telemedicine and diagnostics capabilities.
Healthcare providers need to consistently make excellent operational decisions to become streamlined and cost-effective. Hence, hospitals must establish an effective operational management process through a centralized command-and-control capability. An effective process would ideally be predictive and use optimization algorithms and artificial intelligence to deliver prescriptive recommendations while continuing to learn. The ability to mine and process large quantities of data to deliver recommendations will help streamline hospital operations. Frost & Sullivan believes that the shift to intelligent solutions will increase hospital operational efficiency through predictive analytics to improve the planning and execution of key care delivery processes.
The drive to enhance efficiency and increase surgical output per facility will drive the uptake for digital operating rooms (ORs). The digitization of ambulatory surgical centers and hospitals will create more value-based care and drive revenues for the centers adopting them. The COVID-19 pandemic affected surgical volumes as many elective procedures were put on hold and rescheduled. The increased backlogs will make the need for operational efficiency for hospitals and ORs more urgent since a challenge in terms of resources is also expected. Frost & Sullivan believes that the medical device company’s role will evolve from supplier to partner in healthcare to provide customers with data analytics and predictive capabilities for procurement and inventory management. As payers push for standardization and value in the healthcare system, the benefits of smart and digital ORs will be realized. Building patient confidence comes from ensuring safety from exposure to the virus and reduced costs and procedure time.
The Middle East region is already investing in advanced technology such as robotic surgery. As part of digital transformation initiatives, hospital and operating room digitalization is also beginning. As the region continues to build new healthcare infrastructure (including day surgery centers) to serve remote and semi-urban locations outside major urban centers, “digital” will be embedded in the new setup. This will streamline the adoption of advanced analytics and other solutions for the operating room to improve efficiency. Several solutions are already available in the global market and must be leveraged to address local healthcare challenges. Ultimately, investments in these advanced capabilities will help the region’s population gain from increased access and faster recoveries, helping achieve improved patient outcomes and experiences at lower healthcare costs.
Frost & Sullivan has identified the top opportunities in the digital operating room market:
1. Tele-surgery Enabled with Digital Connectivity, Eliminating Latency.
The accuracy of robotic surgery depends on the image quality that is obtained by the system, dexterity of the robotic arms and tools, and the ability of the system to distinguish between healthy and diseased tissues during surgery. Hospitals and surgery centers will also need to turn the focus on technologies that support telesurgery to nullify the latency issue and leverage the benefits of ultra-high-definition capabilities to deliver high bandwidth and real-time responsiveness with high-definition images. Hence, the focus will shift to capabilities for offering instant connection with specialists, irrespective of location and distance, to collaborate in real time during the surgical operation.
Tele-surgery using robots can also help the Middle Eastern patient population gain access to global surgical expertise, instead of having to fly to western countries. This has the potential to save significant costs incurred by the Middle Eastern governments in ensuring the best possible care for their citizens.
2. Artificial Intelligence for Predicting Surgical Outcomes and Minimizing Variability:
Instead of relying solely on a video feed, artificial neural networks can use online search tools and dig into legacy databases to guide surgeons with information such as the boundaries of a tumor. Investing in robot-assisted surgery for minimally invasive capabilities will benefit patients due to their smaller incisions and quicker healing. Robots with artificial intelligence (AI) are important because they enable the analysis of previously recorded data to inform the surgeon and the team of more effective surgical approaches. With the large volumes of data from endoscopic and laparoscopic surgeries, the future potential builds for AI and machine learning (ML) will help uncover critical insights for surgery. AI and data analytics will help solve the various surgery department challenges. With the help of AI, the best techniques that align with effective outcomes can be identified and applied for optimal resource utilization and cost-effective services.
For example, similar to global markets, the Middle East region is seeing a rise in cancer cases. It is investing heavily in genomics testing capabilities to better understand cancer patterns in the region. As more patient data becomes available, along with clinical literature and insights, offering this data in real-time to surgeons can help improve the outcomes of the surgery, or better yet, help plan it better.
3. Collaboration with Academic Centers:
As learning and teaching are crucial for the medical community, harnessing IP technology becomes even more critical to ensure real-time, high-resolution images and various patient and healthcare content is delivered from the OR to various education platforms. With large volumes of data inclusive of recorded imagery, video, and audio, centers will be required to integrate with smart applications to enable ease of accessibility and for future use. Centers and ORs must invest in technology, providing collaborative benefits. This will ensure the availability of content at any time as per the requirement of the physician or surgeon at home on a desktop or mobile device and even at a medical conference.
As the Middle East region invests in improving the domestic medical education of surgeons, live feeds from the OR (preceptorship, proctorship, and mentorship) will help educate trainee surgeons on the best practices in their chosen field of surgery. Collaborations with international hospitals and surgeons can help democratize access to the best surgeons around the world for local medical students.
Medical device companies will aim to partner with payers, providers, and technology companies to help synergize comprehensive products and services to a larger customer base. The focus will be to expand their portfolios by adopting a patient-centric approach in the diagnosis, detection, treatment, and post-care to cater to solutions across the value chain and be a single-stop-shop provider to attract customers and collaborate with other companies that can complement their capabilities.
About Frost & Sullivan
For over six decades, Frost & Sullivan has helped build sustainable growth strategies for Fortune 1000 companies, governments, and investors. We apply actionable insights to navigate economic changes, identify disruptive technologies, and formulate new business models to create a stream of innovative growth opportunities that drive future success. For more, visit www.frost.com.
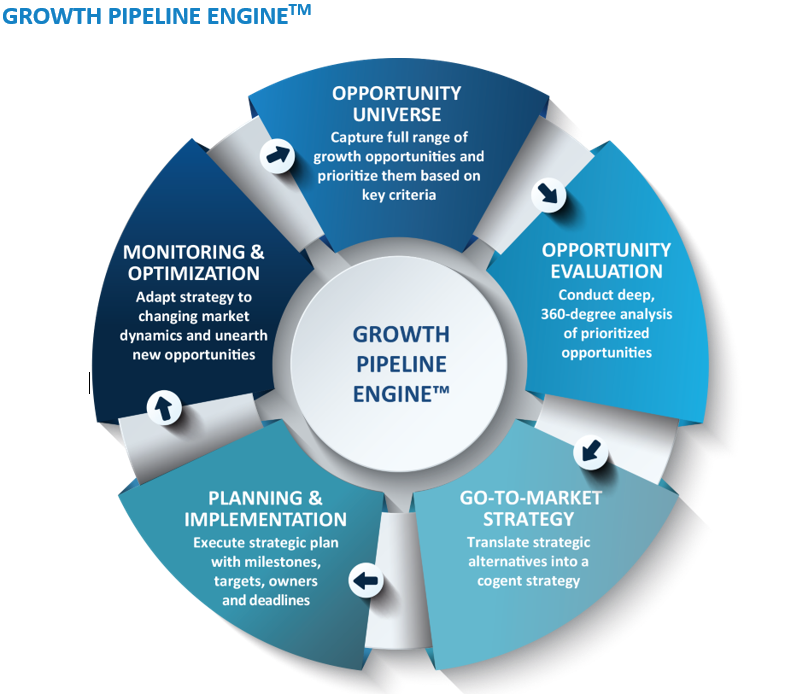
AFrost & Sullivan’s Growth Pipeline Engine™ supports clients through all phases of growth — Developing, evaluating and prioritizing opportunities, building and implementing go-to-market strategies, and optimizing opportunities. The objective is to be a client’s first step on their growth journey.
For more information, write to: [email protected]