Innovations in Surgical Management of Gastroesophageal Reflux Disease
13 January 2019
By George W. Holcomb III, MD, MBA, Children’s Mercy Kansas City, Kansas City, Missouri, U.S.
Gastroesophageal reflux symptoms are common in infancy, childhood, and adolescence. In one study, 2-7 per cent of parents of 3 to 9-year-olds report their child experienced heartburn, epigastric pain or regurgitation within the previous week, whereas 5-8 per cent of adolescents reported similar symptoms.
Most children respond well to changes in their diet, as well as medical management for these symptoms. Gastroesophageal reflux disease, (GERD), is a more serious condition and has an incidence of 1.5 cases per 1,000 person-years in infants, declining until 12 years of age, and then peaking at 16 to 17 years of age (2.26 cases in girls and 1.75 cases in boys per 1,000 person-years in 16- to 17-year-olds). Overall, the childhood prevalence of GERD is estimated at 1.25 to 3.3 per cent, compared with 5 per cent among adults.
GERD can affect a child’s growth and development, and can lead to more serious complications, such as vomiting and damage to the oesophagus. At Children’s Mercy Kansas City, the Division of Pediatric Gastroenterology is performing cutting-edge research into the pharmacological management of GERD, but some children do not respond well to medical treatment.
In refractory cases, surgery may be the best treatment option. With nearly 20 years of experience in the use of laparoscopic fundoplication for the management of gastrointestinal reflux, the general surgeons at Children’s Mercy have published a number of articles on this technique.
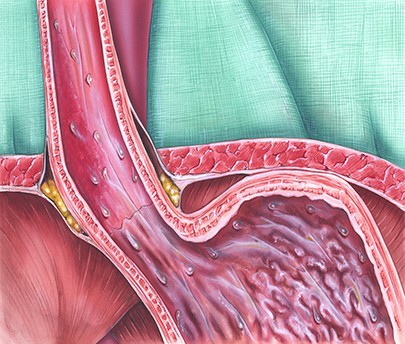
Specifically, the Nissen fundoplication is our preferred operative approach to treating GERD. This procedure was named after Dr. Rudolf Nissen, the surgeon who developed it in the 1950s. Since that time, the surgery has evolved from an open procedure that required large incisions to a laparoscopic, or minimally invasive, procedure.
One of the areas of focus among the general surgeons at Children’s Mercy is how to prevent transmigration of the fundoplication wrap following performance of a Nissen fundoplication. We have studied this problem carefully and scientifically, initially through a retrospective study, which was followed by two prospective clinical trials evaluating differences in the operative technique.
In the last prospective clinical trial, which was published in the January 2018 issue of the Journal of Pediatric Surgery (53:25-29, 2018), the Children’s Mercy surgeons found that limited dissection of the oesophagocrural junction and limited mobilisation of the oesophagus resulted in none of the 120 patients enrolled in the study developing transmigration of the fundoplication wrap in the postoperative period with a median follow-up of four years.
The goal for this, and all, research performed by the Department of General Surgery at Children’s Mercy, is to determine the effectiveness and practical application of utilising this specific surgical technique to improve outcomes for patients. This study concluded when minimal pharyngoesophageal dissection is performed, oesophagocrural (EC) sutures offer no advantages and increase operating time. Thus, our surgeons confirm that the pharyngoesophageal membrane should be kept intact, which results in minimal dissection around the gastroesophageal junction.
Paving The Way
The paediatric general surgeons at Children’s Mercy Kansas City have been early adopters of minimally invasive technology and techniques. In 1999, Children’s Mercy established the Center for Minimally Invasive Surgery, designed to make state-of-the-art minimally invasive surgeries available to paediatric patients across the globe.
Center for Prospective Clinical Trials Investigates Paediatric Surgical Questions
The Center for Prospective Clinical Trials within the Department of Surgery at Children’s Mercy Kansas City was e0stablished in 2006 to perform randomised studies investigating variables that do not allow the patient’s course to vary from normal daily practice. The centre also performs prospective observational studies.
All of the studies performed in the centre are protocolised care based on evidence and outcomes, which are institution-specific. The hospital’s randomised data are exactly what the provider can expect in terms of outcomes for patients they refer for surgery at Children’s Mercy. The centre’s goal is to address the many questions common to paediatric surgery.
Paediatric Surgical Care
Children’s Mercy is one of only 10 centres in the U.S. to be verified as a Level 1 Children’s Surgery Center, the highest rating possible from the American College of Surgeons, which has set the highest standard of care in the U.S. By joining this group of Level 1 Children’s Surgery Centers, the hospital is contributing to the innovation of paediatric surgery, which impacts the lives of children around the world.
The review process to become verified is rigorous and stringent, including a thorough site visit by an ACS team of surveyors who review the hospital’s structure, process, and clinical outcomes. The team, which consists of experienced paediatric surgeons, anaesthesiologists and nurses, visit all areas of the hospital to make sure the people, resources, the culture of safety, and administrative support ensure patients receive the highest level of care.
An important component of providing this level of surgical care is expertise. At Children’s Mercy, only experienced paediatric anaesthesiologists care for each child. This ensures the patient has a safe and smooth anaesthetic experience.
In fact, the paediatric anaesthesiologists at Children’s Mercy administer anaesthesia for more than 27,000 children each year — that’s 74 each day. Most adult hospitals only treat about 200 children each year–less than one a day.
Surgical Expertise
At Children’s Mercy, 20,144 surgeries were performed in fiscal year 2018. This team’s surgical expertise extends to a number of conditions commonly seen in the paediatric population. These include:
- Center for Pectus Excavatum and Pectus Carinatum, which offers minimally invasive surgery for pectus excavatum, and the largest experience in the U.S. with the dynamic compression device bracing system utilised for pectus carinatum.
- Same-day surgery for non-perforated appendectomy.
- Laparoscopic inguinal hernia repairs performed on an outpatient basis at Children’s Mercy Hospital Kansas or at the Children’s Mercy Kansas City Adele Hall campus.